One Year with COVID: New Orleans’ COVID Successes and Opportunities for Increasing Health Equity
Published: Apr 08, 2021
COVID-19 took the world by surprise in late 2019. While there were a few reported cases in the United States when the 2020 Mardi Gras season rolled around, the thought of canceling Mardi Gras was far from even the CDC’s mind. We now know that carnival events resulted in one of the earliest and fastest growing outbreaks in the country. The first documented COVID-19 related death in New Orleans was on March 14th, 2020. Over the next three months, at least 495 New Orleanians would die of COVID.
The New Orleans metro area was hit hard in those early days, but the more we learned about the virus, the better we got at mitigating its effects. Outbreaks in nursing homes and other long-term care (LTC) facilities were identified rather quickly and better contained. Widespread masking contributed to declining fatalities overtime. Initial lockdown restrictions were hard on everyone, especially restaurants and bars, but they proved to be an efficient tool to reduce transmission and save lives. Later, as decisionmakers tried to strike a balance between economic damage, restrictions on personal behaviors, and health risks, more lenient policies were less effective in mitigating a third wave of COVID cases and deaths.
All vaccines available to the public thus far are free, safe, and 100 percent effective at preventing hospitalization and death from COVID-19.
Today, vaccines offer a critical opportunity to eliminate deaths and hospitalizations and potential pathway out of sometimes frustrating, but necessary, coronavirus restrictions. Still vaccination rates among Black New Orleanians remain disproportionately low. Attention must be paid to inadvertent racial inequity embedded in vaccine distribution plans. Well-informed and resourced outreach and distribution will be required to overcome the remaining obstacles to equitable vaccine accessibility.
A year in three parts
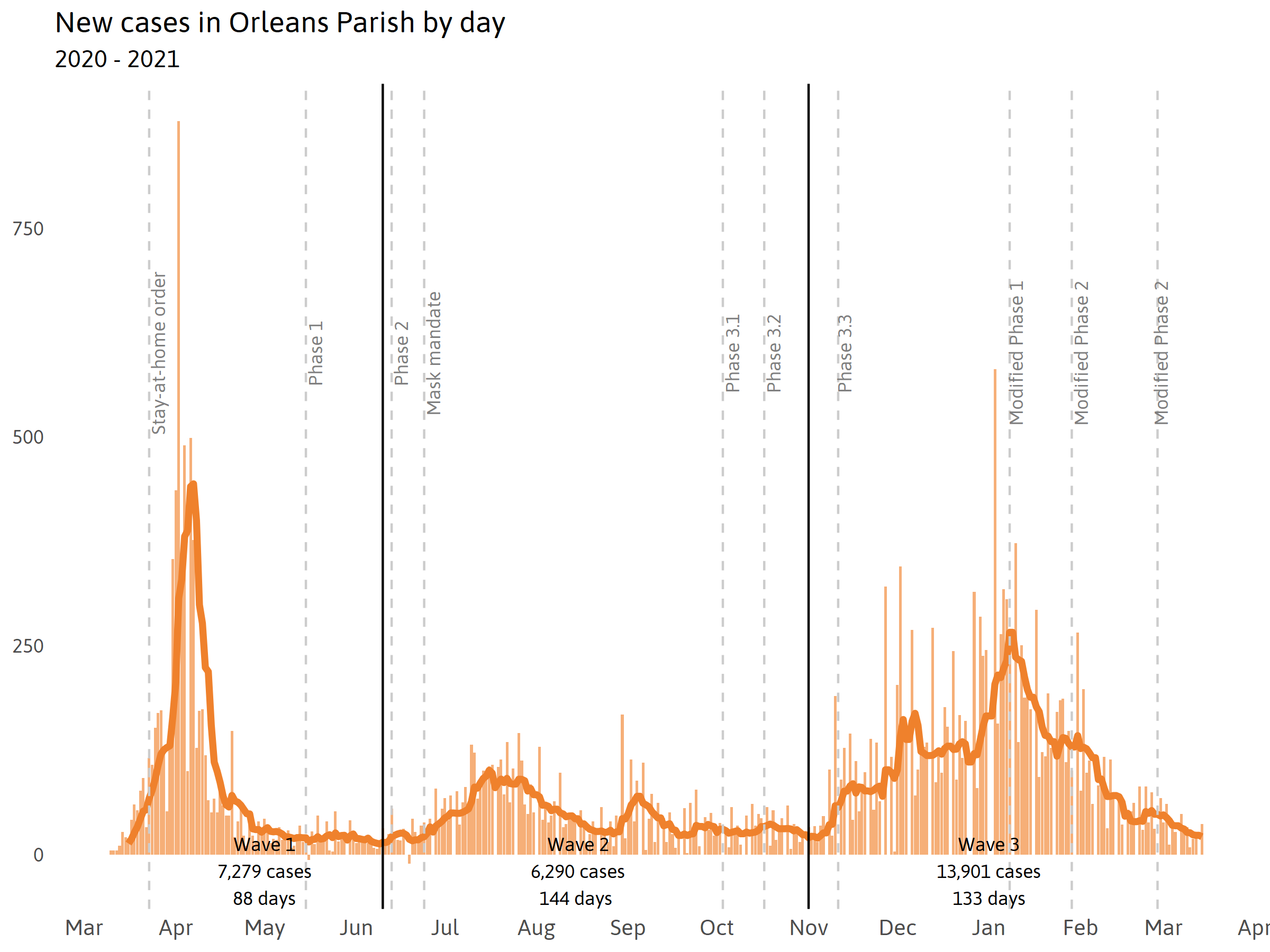
New Orleans’ first year with COVID can be analyzed in three major waves:
- the initial onslaught of (documented) cases and deaths from March 14 to June 10, 2020;
- after successfully flattening the curve, a rise in cases as policy-based restrictions loosened from June 11 to November 1, 2020; and
- a significant swell in cases and deaths during and after the late 2020 holiday season from November 2 to March 14, 2021.
By dissecting these three distinct outbreaks, we point to policies and interventions that helped reduce the impact of the COVID-19 pandemic in New Orleans.
The first case of COVID-19 in New Orleans has been linked to a domestic traveler entering the city in mid-February 2020. New Orleans, having not been alerted to an imminent threat, proceeded with carnival activities without precautions two weeks later. It is now understood that many Mardi Gras festivities likely spread COVID across the city and resulted in one of the earliest and fastest growing outbreaks in the country. As soon as testing capacity expanded, it was clear that COVID was infecting and killing residents at an extremely high rate.
On March 20th, Mayor LaToya Cantrell issued a strict stay-at-home order. Soon after, cases and deaths quickly declined. It was 92 days from the first documented case of COVID in the city on March 14th until the next wave emerged on June 10th. During this time there were 7,247 documented cases and 495 documented deaths, making for the highest ratio of deaths to cases of all three outbreaks. From May to mid-June the curve flattened in New Orleans, Mayor Cantrell reopened businesses to a Phase 1 setting on May 15th, then Phase 2 on June 13th, 2020.
The 144 days between June 10th and November 1st, constituting the second wave, saw relatively fewer cases and deaths in the city. During this time, there were 6,290 documented cases and 48 documented deaths. All told, only a tenth as many people died in the second wave as the first wave. In anticipation for the July 4th weekend, Mayor Cantrell issued a city-wide mask mandate in New Orleans on June 24th. Still, cases rose in response to activities related to the holiday weekend.
The third and final outbreak in New Orleans from November 2nd to March 14th, 2021 lasted 133 days and saw 13,960 new cases and 121 deaths. As before, leaders attributed rising cases and deaths during this time to holiday travel and gatherings. During this phase, the Mayor enacted modified Phase 1, modified Phase 2, and modified Phase 3 policies which did not control spread of the virus as effectively as the policies enacted during the first outbreak. Elevated cases and deaths lingered for months, resulting in more than double the number of cases and deaths as the second outbreak.
During the first wave, 1 in 15 people who tested positive for COVID-19 died from the virus. By the third outbreak, that changed to only 1 in 122. There are several reasons for this impressive decline in fatalities, including ramped up testing, improvements in prevention, improvements in treatment, and infections shifting from older populations to younger populations.
The first case of COVID is estimated to have entered New Orleans in mid-February, but it was not until late April that testing became widely available. Because testing capacity had not yet ramped up to meet demand, only people with symptoms were eligible to be tested early on in the pandemic. However, many individuals were infected but not counted among the official cases because they had no symptoms and thus were never tested. A study conducted by Ochsner during that time revealed that 40 percent of all infected people never experienced symptoms. COVID deaths, in contrast, are less likely to be under counted. Thus, the ratio of COVID deaths to cases was higher during the first outbreak, in part due to severely inaccurate data on the total number of cases.
Widespread mask-wearing reduced the number of overall cases by preventing transmission. It also reduced the number of severe cases by limiting the amount of virus people were exposed to. Reducing the number of cases that required hospitalization in turn helped to save lives by freeing up medical resources for those who were severely ill.
Lifesaving improvements in treatments and therapies also resulted in shorter hospital stays and fewer deaths. Notably, the use of ventilators declined in late April of 2020 when a study found that using ventilators did not save lives except for in the most acute COVID cases. In October 2020, the U.S. Food and Drug Administration approved the first therapeutic drug treatment for COVID-19, which contributed to saving lives.
Finally, the share of cases that resulted in death fell in New Orleans because the elderly, who are more likely to die if infected, comprised a smaller proportion of overall cases over time. During the first outbreak when fewer people were aware of the risks, 16 percent of all infections occurred among people 70 years and older and 13 percent occurred among people 18 to 29 years old. By the second wave, only 6 percent of all cases were among those 70 and older, while 29 percent of all cases were among 18- to 29-year-olds.
The reason for the decrease in cases among elderly residents is likely two-fold. After the first outbreak, elderly residents were more aware of the risks COVID posed to them and were better able to protect themselves. In fact, the COVID Impact Survey conducted from April to June of 2020 found that nationwide people 60 years and older were the most likely of all age groups to adhere to mitigation behaviors recommended by the CDC. In addition, COVID cases among elderly living in nursing homes and long-term care facilities decreased significantly over time.
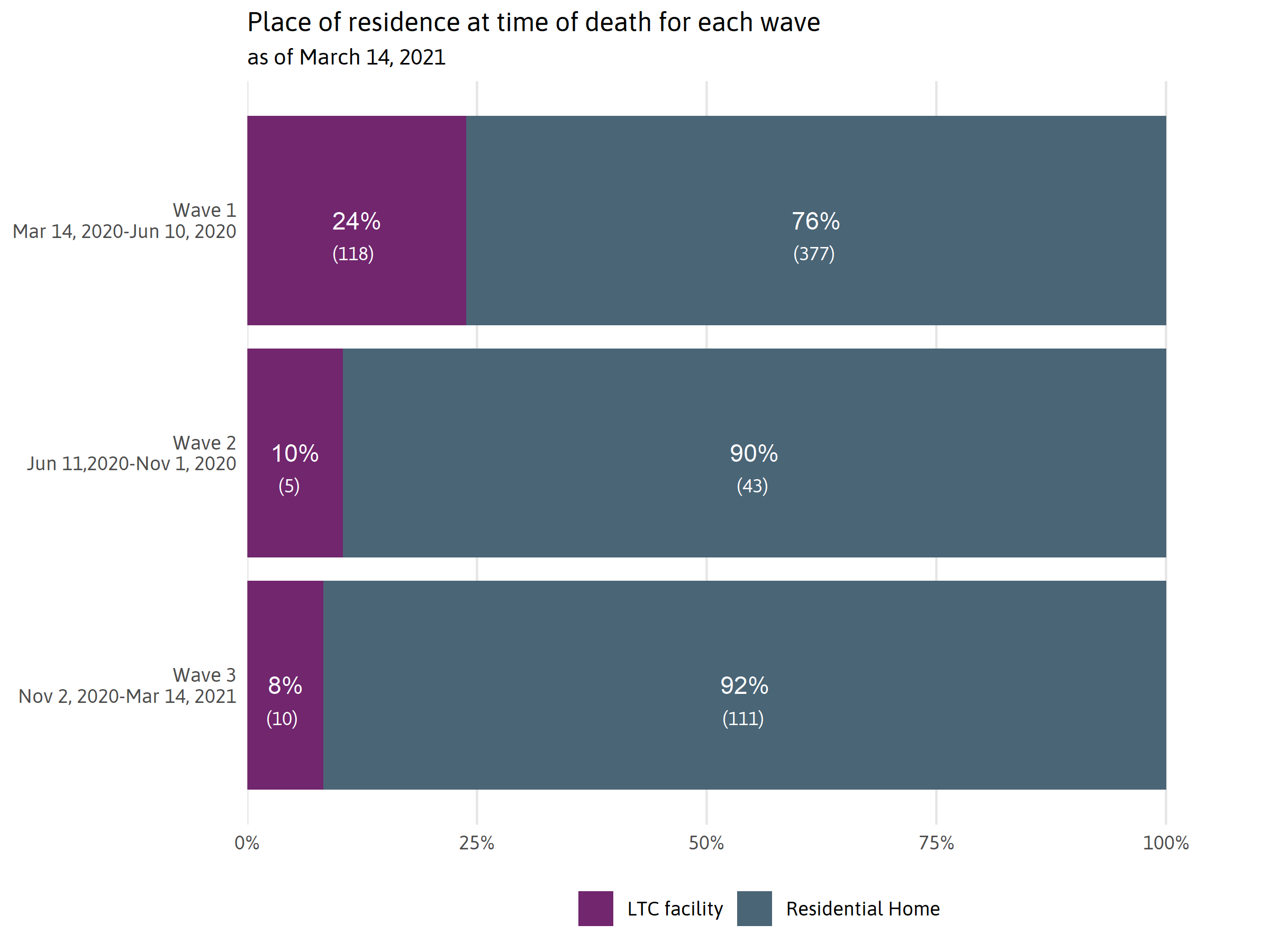
Successes over the past year
Nursing homes were severely impacted by the COVID-19 pandemic. However, through universal testing, visitor restrictions, and the use of personal protective equipment, spread was largely contained. In addition to successful infection control, residents and staff of long-term care (LTC) facilities were among the first to be prioritized for the COVID-19 vaccine during the latter part of the year. In New Orleans, 24 percent of all COVID deaths during the first outbreak were among LTC facility residents. By the third wave, LTC facility residents were only 8 percent of all deaths in the city.
The racial composition of nursing homes differs from the general population of New Orleans. Nursing home residents tend to be more White. This may be because institutionalized care of the elderly is more common among White families than Black in New Orleans. According to the 2010 Census (the most recent available data on the racial make-up of group home populations), White people 65 years and older in New Orleans were twice as likely as Black people 65 or older to live in a group home setting such as a LTC facility.
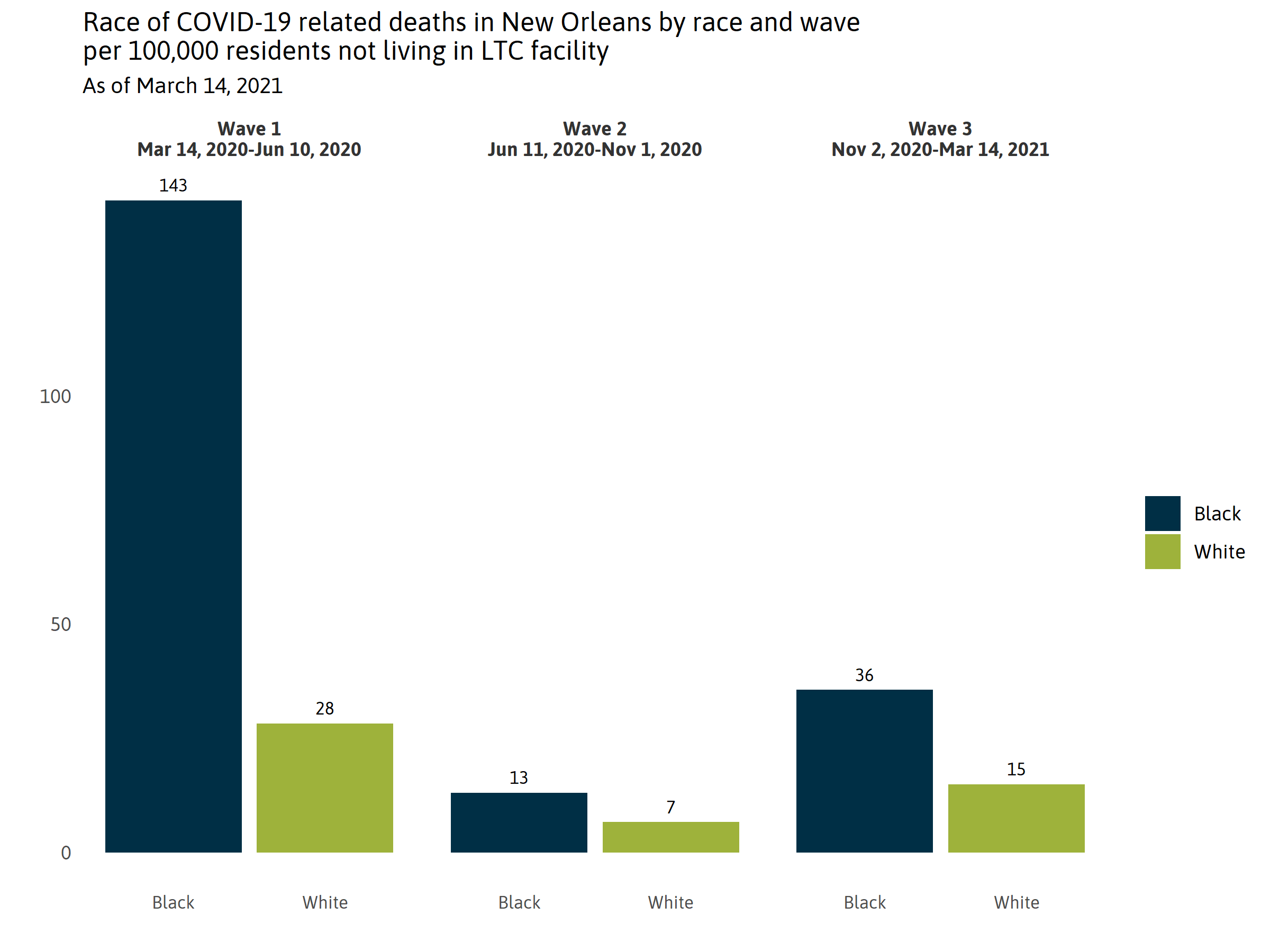
Examining trends in COVID deaths — excluding nursing homes — is important for assessing the overall effectiveness and equity of New Orleans’ COVID mitigation strategies. During New Orleans’ first year with COVID, Black New Orleanians outside of LTC facilities died over three times the rate of White New Orleanians, even after accounting for the larger Black population in New Orleans. Outside of LTC facilities, New Orleans lost 441 of its 230,418 Black residents to COVID as of March 14th, 2021, compared to 60 of its 120,582 White residents. But as understanding of the risks, science of transmission, and effectiveness of prevention measures evolved, racial disparities decreased in New Orleans. During the first outbreak, there were 143 COVID deaths for every 100,000 Black New Orleans residents – five times higher than the White COVID death rate – but the gap was half that by the third outbreak. While the exact reasons for this decline have not been studied, a July 2020 survey found that New Orleans had the highest rate of mask wearing among all Louisiana parishes. The high rate of Black deaths in New Orleans early in the pandemic may have contributed to high motivation among Black New Orleanians to adhere to mask mandates and social distancing guidance.
National research indicates that people of color have been more likely to adhere to social distancing and masking guidelines, but they are also less able to avoid high-risk settings. As recently as late February, 2021, according to the Census Bureau’s Pulse survey, 30 percent of White Louisiana households had at least one adult able to substitute telework for in-person work, compared to only 15 percent of Black households and 14 percent of Hispanic households.
Health equality versus health equity
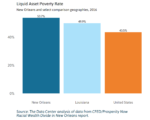
The impact of COVID-19 has not been felt evenly across New Orleans. Black New Orleanians have been disproportionately impacted. However, the vaccine introduces an important opportunity to close COVID related health disparities.
Vaccine equality would ensure vaccines are distributed proportional to the racial make-up of the total population.
Vaccine equity would prioritize outcomes such that those most impacted by COVID would be prioritized, with the aim of eliminating resulting COVID health disparities.
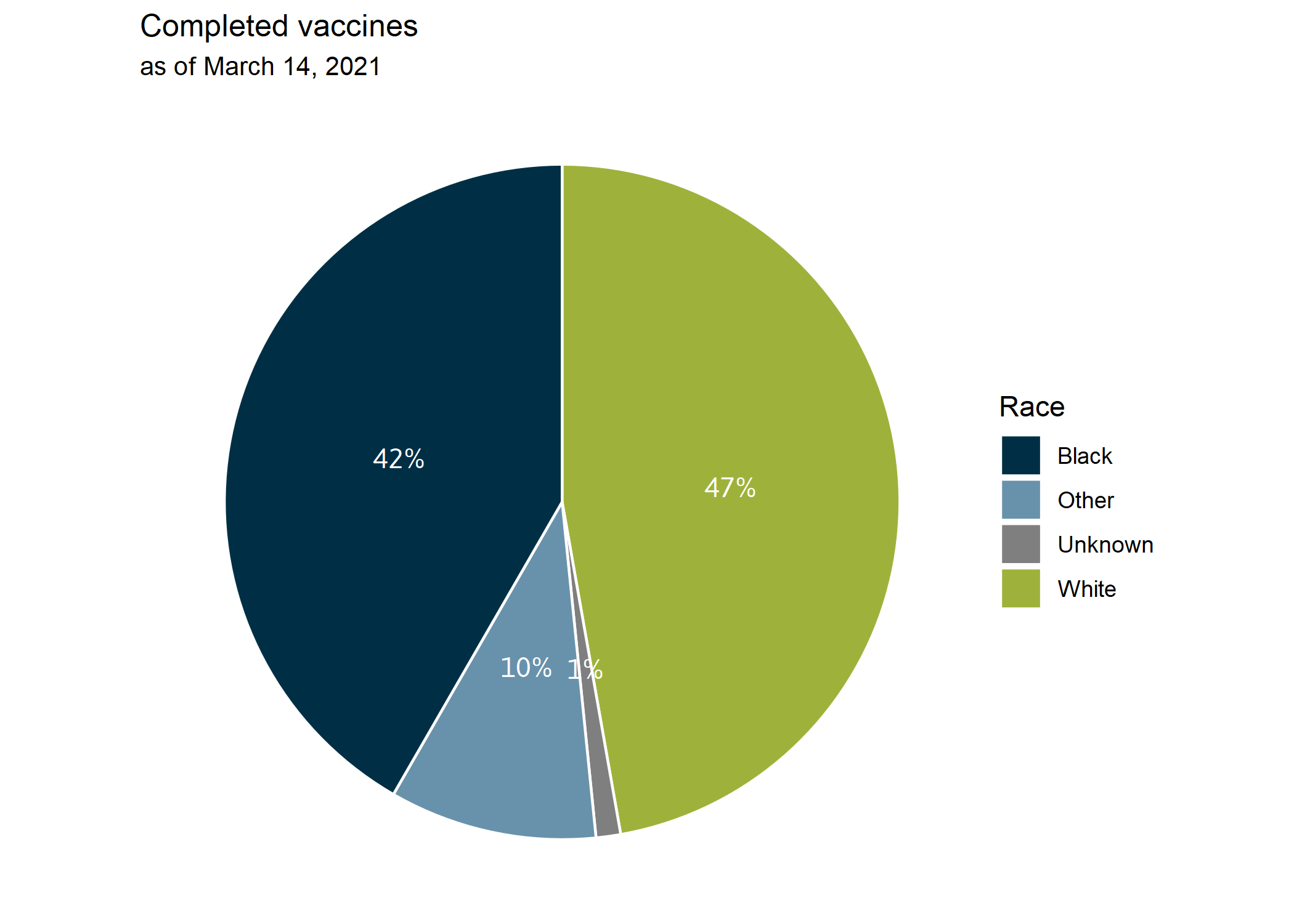
As of this writing, Black New Orleanians have had higher rates of infection, hospitalization, and deaths from COVID but have also received proportionally fewer vaccines. In New Orleans, 59 percent of the population is Black, 75 percent of COVID deaths have been Black people, but only 42 percent of people who have been fully vaccinated against COVID were Black. For now, New Orleans has achieved neither equal nor equitable vaccine distribution.
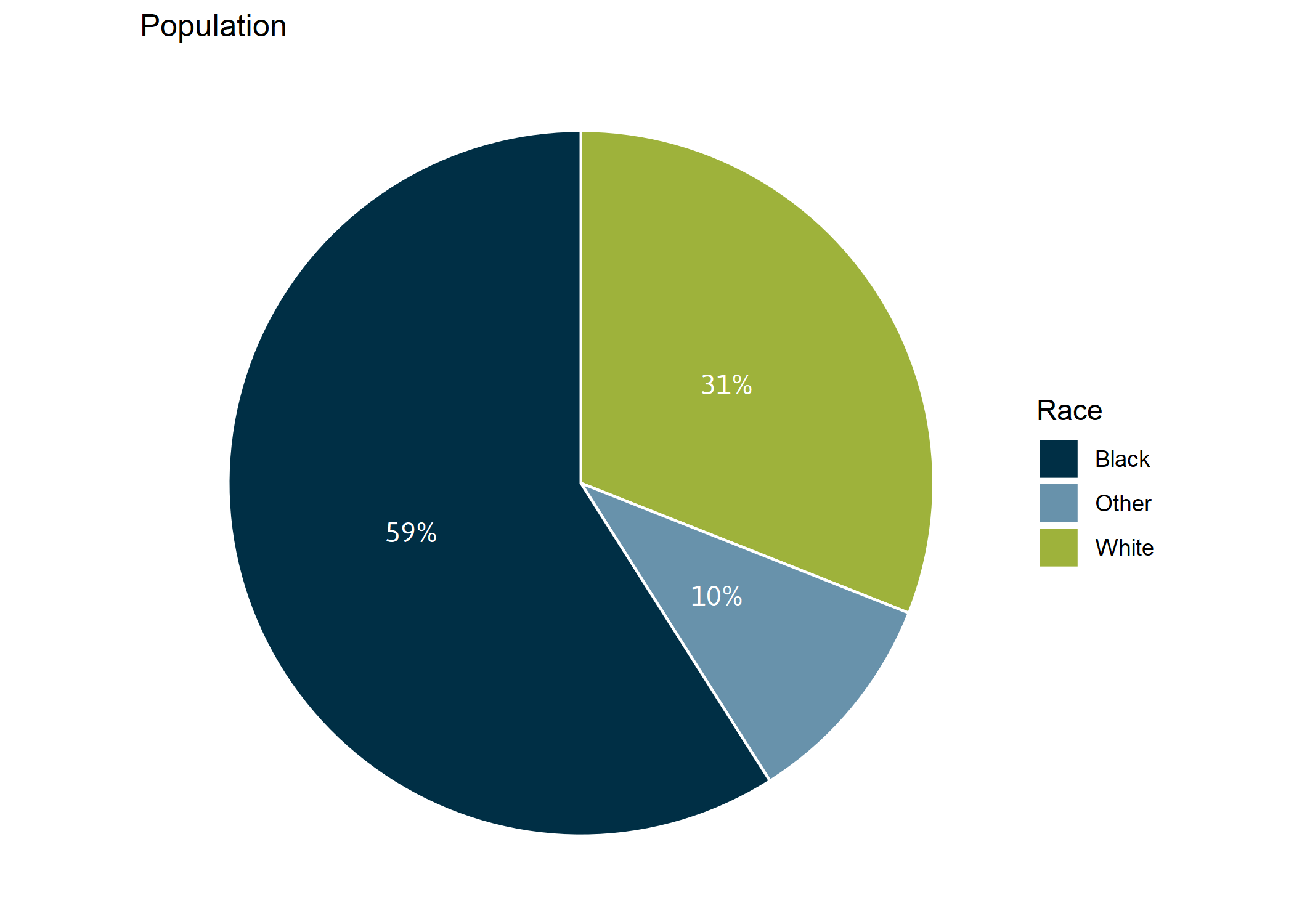
Note: “Other” includes Asian, American Indian, people who identified as two or more races, Hispanic/Latino, and other race/ethnicities.

Note: “Other” includes Asian, American Indian, people who identified as two or more races, Hispanic/Latino, and other race/ethnicities.
Note: “Other” includes Asian, American Indian, people who identified as two or more races, Hispanic/Latino, and other race/ethnicities.
There are several reasons why Black New Orleanians have not received their fair share of vaccines thus far. Everyone in Louisiana over the age of 16 is now eligible to receive the vaccine. However, vaccine eligibility criteria set by the state did not strongly enough prioritize those most impacted by COVID in New Orleans. And efforts to date to reach all of the most impacted populations have not been sufficient to reduce health disparities.
When early vaccine prioritization groups were limited to nursing home residents, elderly Black residents who receive care at home were excluded. However, during Phase 1A the vaccine became available to people outside of nursing homes who were 70 years or older. In Phase 1B the age criteria was lowered to 65. But because Black New Orleanians in the non-nursing home population tended to die from COVID younger than their White counterparts, these criteria disproportionately included the most vulnerable White New Orleanians but failed to also prioritize the many Black New Orleanians 60 years or older who were clearly similarly vulnerable to COVID. This mismatch between state policy and local outcomes is evident in data from the Coroner’s office on COVID death statistics.
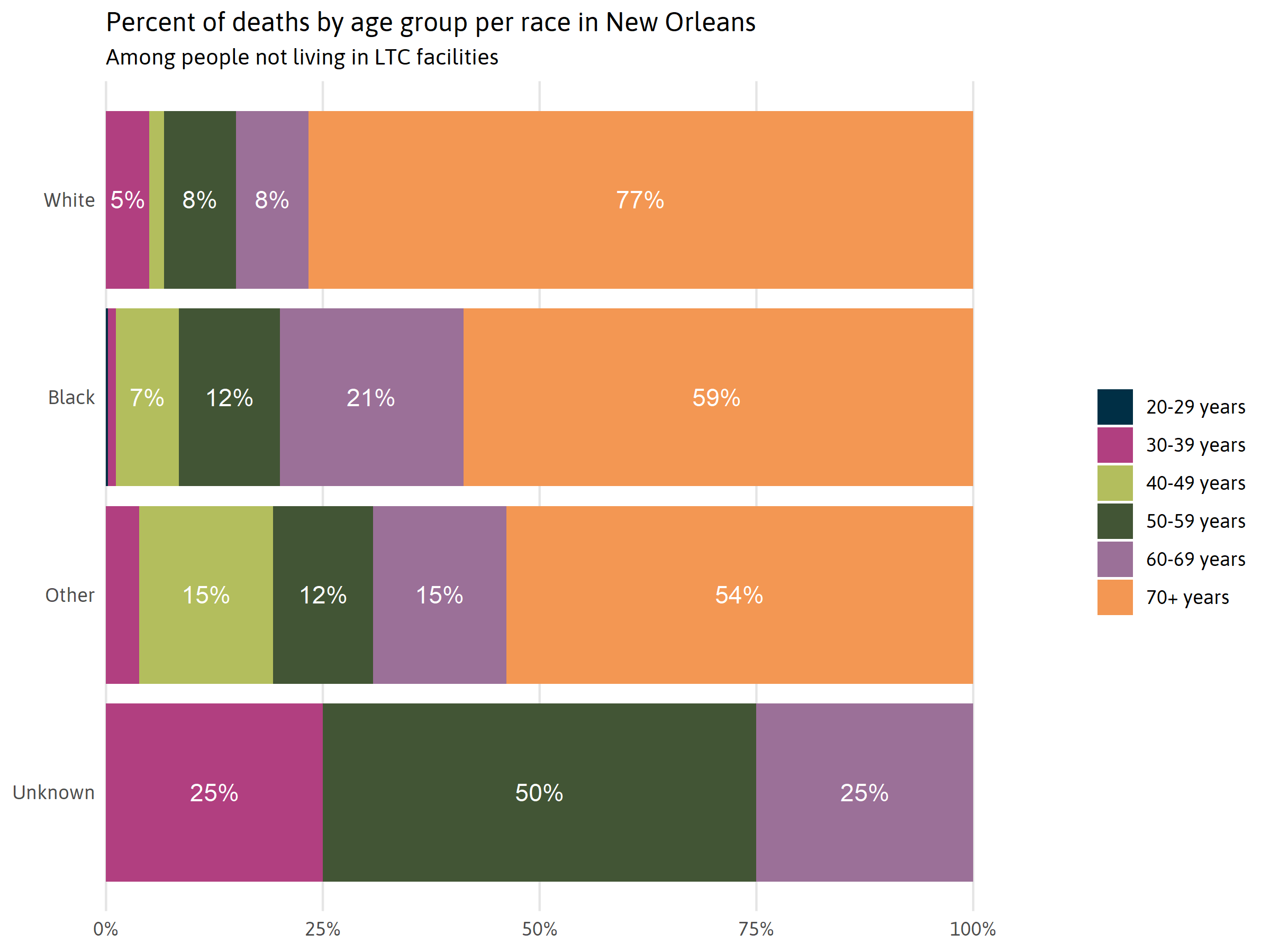
Note: People living in LTC facilities were excluded from this graph because they were already eligible for the vaccine, regardless of their age.
Applying the vaccine in an ex post facto simulation to what we now know about those most vulnerable to COVID (as indicated by the age and race of those who died in the first year) we can see that:
- Phase 1A criteria would have made the vaccine available to 77 percent of the White New Orleanians who died of COVID but only 59 percent of all Black New Orleanians who died from the virus.
- Phase 1B criteria would have made the vaccine available to 83 percent of the White New Orleanians who died of COVID but only 71 percent of the Black New Orleanians who died.
- The Black-White disparity virtually disappears when the age-based vaccination criteria drops to 55 years or older, with no preexisting conditions. This criteria would have made the vaccine available to 88 percent of the White New Orleanians who died of COVID and 87 percent of the Black New Orleanians who died.
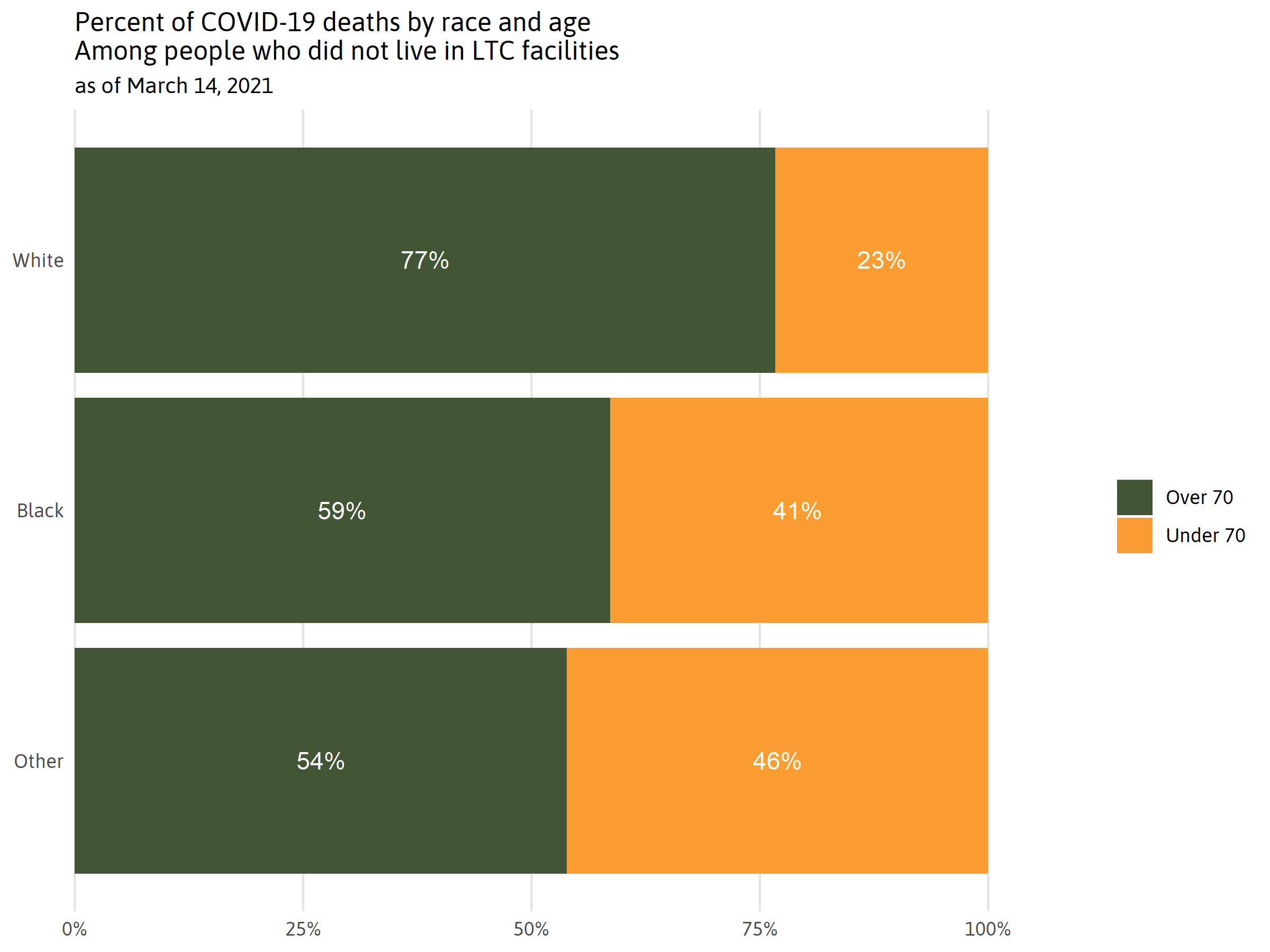
Note: People living in LTC facilities were excluded from this graph because they were already eligible for the vaccine, regardless of their age.
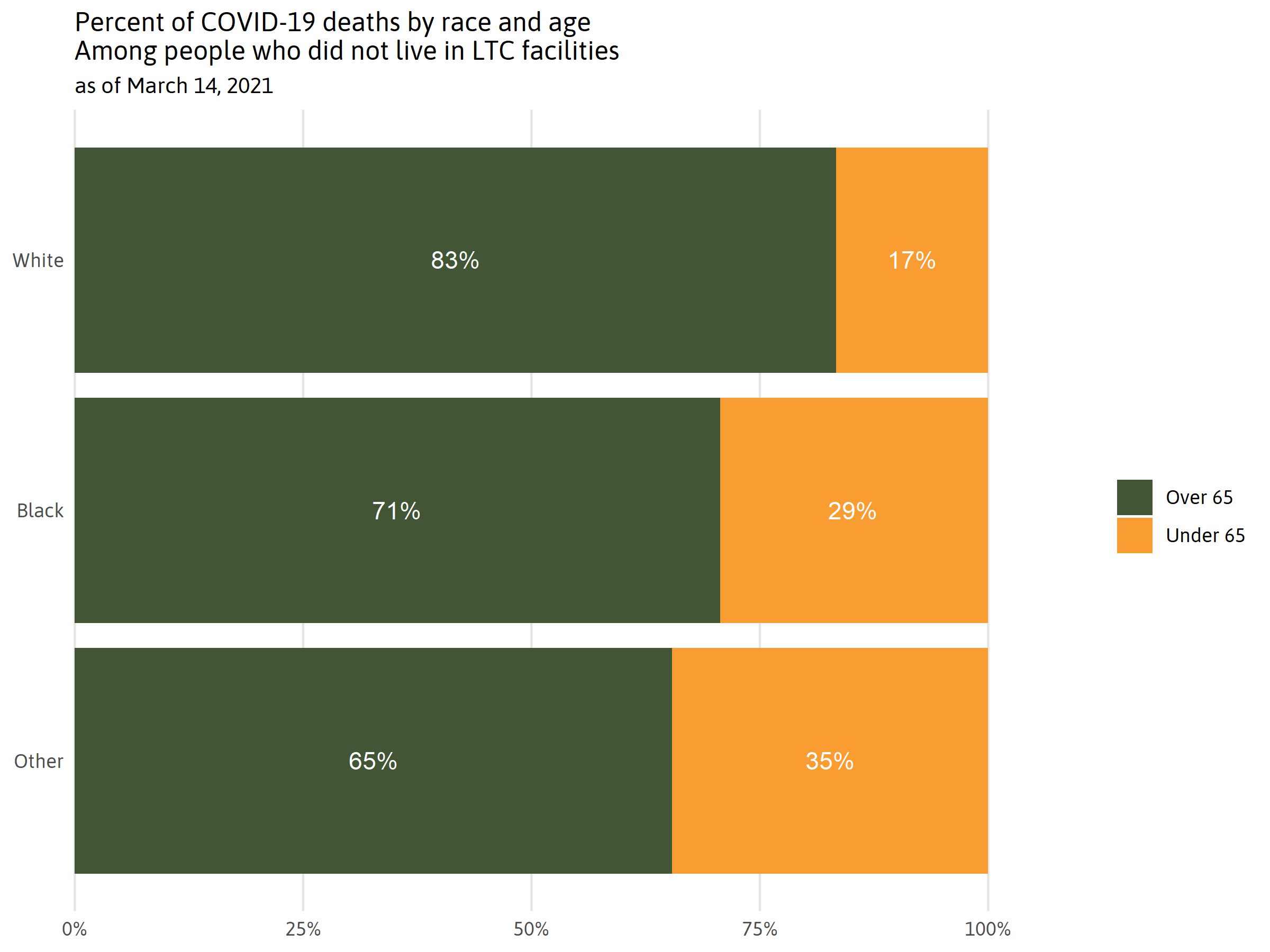
Note: People living in LTC facilities were excluded from this graph because they were already eligible for the vaccine, regardless of their age.
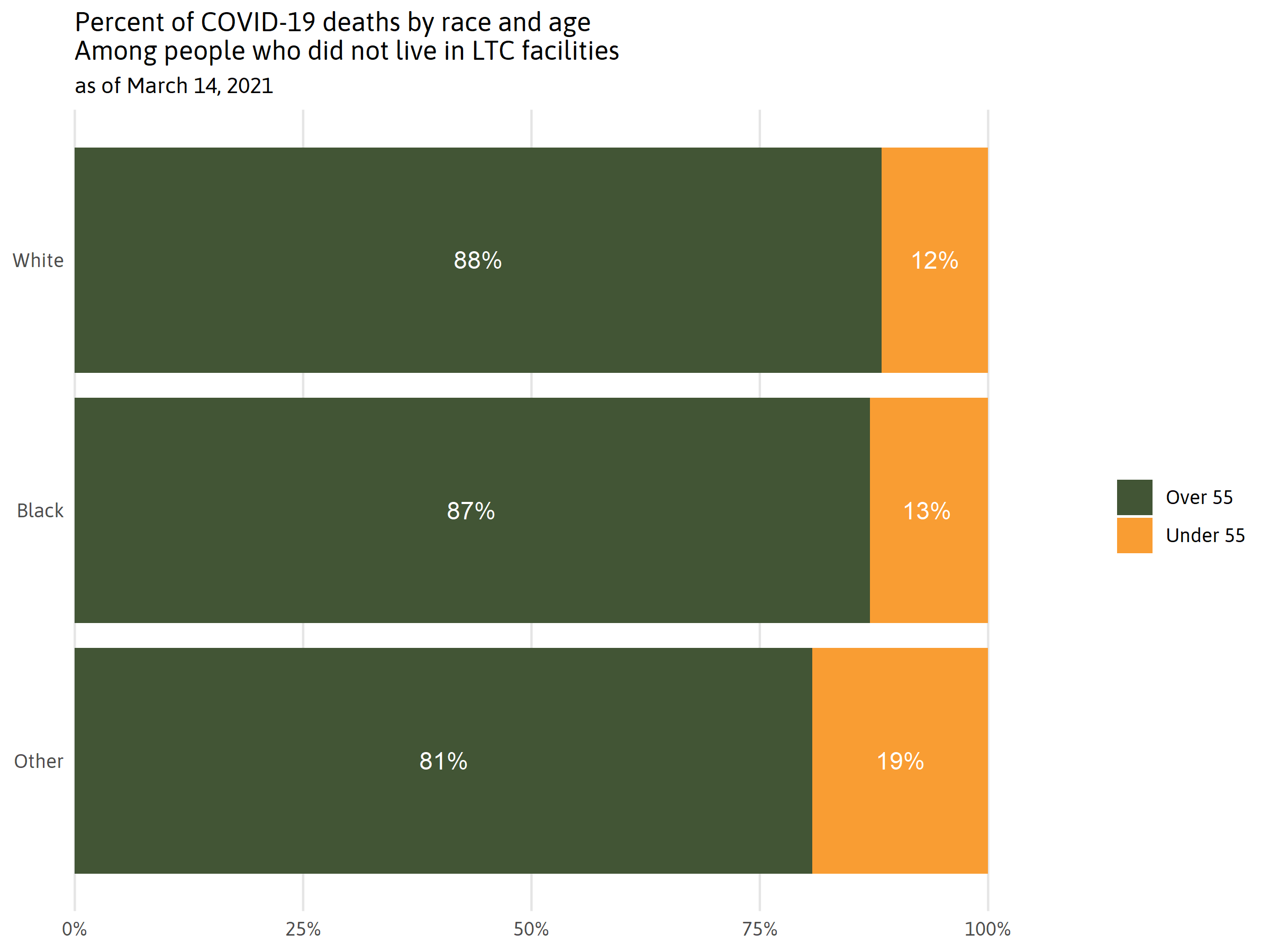
Note: People living in LTC facilities were excluded from this graph because they were already eligible for the vaccine, regardless of their age.
Besides nursing home residents and the elderly, several occupations were prioritized in Phase 1A and 1B. But these prioritized occupations including teachers, police officers, dentists, and EMTs are more likely to be White in New Orleans than overall city demographics. Meanwhile, other essential workers who are majority minority were not prioritized until the last priority group, Phase 1B, Tier 2. As one example, butchers and meat, poultry and fish processing workers in Louisiana are 47 percent Black and 11 percent Hispanic. These workers are essential to keeping our grocery stores stocked, and are among a larger group of food processing workers who have suffered the largest number of outbreaks and resulting infections of all other non-congregate settings as identified by Louisiana Department of Health contact tracers. Indeed, these workers hailed as “essential” throughout the pandemic, were given access only after Louisianans 16 years and older with pre-existing conditions — conditions which included a relatively low Body Mass Index for which the majority of Louisiana adults qualify. Moreover, adults with preexisting conditions were not required to provide proof of their condition. But when essential workers were finally made eligible, they were required to provide proof of their occupation.
Increasing equitable distribution of the vaccine
Now that vaccines are available to all residents 16 years and older in Louisiana, to eliminate COVID health disparities in New Orleans, leaders must execute outreach and distribution plans that overcome common obstacles for New Orleanians who have suffered the most from the COVID-19 pandemic.
Vaccine appointments made online and scheduled during working hours at a downtown or drive-up location, for example, are not likely to be accessible for many New Orleanians. Fully 1 in 5 households in New Orleans do not have access to a car. And nearly 80 percent of New Orleanians who depend on public transportation to get to work are Black, meaning they are less likely to have dependable transportation to get to an appointment. In New Orleans, more than 10 percent of Black households do not have a computer, compared to 1.8 percent of White households. Black families without computers may struggle to schedule vaccine appointments online. Half of all Black families in New Orleans earn less than $25,000 and many of them work in essential jobs in healthcare, retail, and hospitality where work schedules may be unpredictable. Finally, lack of childcare may be an obstacle for parents and guardians juggling work and parenting responsibilities.
Vaccine hesitancy will also need to be addressed. While vaccine hesitancy among African Americans has been a focus of media attention, age may be a greater factor in COVID vaccine hesitancy. March, 2021, data collected by the Census Bureau’s Pulse survey found that 22 percent of African Americans nationwide indicate they “probably or definitely won’t” get the vaccine but a slightly larger share (23 percent) of adults aged 18 to 39 “probably or definitely won’t” get the vaccine. It’s important to note that a person who indicates they “probably or definitely won’t” get the vaccine does not necessarily indicate they are hesitant. They may have concluded they won’t get the vaccine because of obstacles to accessing an appointment, concerns about having flu-like symptoms for a day or two after the vaccine, or a misconception that the vaccine will cost money.
A recent survey by the Louisiana Public Health Institute found that, for both Black and White Louisianans, COVID vaccine willingness is highest for older folks, and hesitancy is greatest among adults aged 18 to 44. Among those hesitant or unwilling to get a vaccine, concern about side effects and the safety of the vaccine were the top reasons. And those who are unwilling to get a vaccine acknowledge that their primary source of information about the vaccine is social media. These folks indicated they would like more information about side effects and safety and would find it most credible if they heard it from doctors and healthcare providers.
Leaders can use these powerful recent survey results to carefully craft and target their vaccine campaign efforts. Many folks are hesitant to get the vaccine because they anticipate flu-like symptoms that can knock them out for a day or two. Clinical trials confirm that vaccine side effects are often more severe for younger adults. Indeed, during clinical trials, patients were advised to take a day or so off from work after being vaccinated in case of side effects such as fatigue — which 44 to 68 percent of patients experienced. Younger adults, sometimes busy with parenting responsibilities and inflexible work schedules or lacking paid sick leave, may find it very difficult to carve out the downtime needed to bounce back from the vaccine. And facing relatively low COVID mortality rates, younger adults may understandably conclude that getting vaccinated is not the highest priority among their many pressing responsibilities, particularly if it may make them feel sick.
Importantly, African Americans comprise the majority of younger adults 20-49 in New Orleans. Addressing concerns of younger adults may be key to achieving equitable vaccine distribution in New Orleans.
Conclusion
While the previous year was difficult in ways no one could have prepared for, New Orleanians still had some successes worth noting. Over the course of the pandemic, the City of New Orleans has maintained more restrictive guidelines than the state as a whole. These have been important for reducing deaths in New Orleans overtime. Still there is more room for improvement as Black New Orleanians continue to die from COVID at a disproportionately high rate. Vaccine distribution continues to provide opportunities to increase equity.
Now that the vaccine is available to nearly the entire population, New Orleans can advance equitable vaccine distribution by identifying and addressing logistical obstacles. New Orleans has already taken important steps to reduce barriers to accessing the vaccine. Free Uber and public transit rides to vaccine events have helped overcome transportation obstacles for many folks. EMS professionals are providing vaccines to all New Orleanians who are homebound.
Churches and community organizations have long leveraged New Orleans’ cultural traditions like fish fries on Lenten Fridays to both satisfy community needs and draw residents toward helpful resources. Some organizations have employed these same traditions to put vaccines within reach of local communities. Taping into New Orleans’ many cultural traditions, especially during Spring months when the weather is most conducive for outdoor events, could quickly expand vaccine distribution to those who are least likely to otherwise receive them.
Understanding, addressing, and targeting vaccine hesitancy among younger adults may improve equitable uptake overall. Institutions and employers that interface with younger adults will be important for reaching this hesitant population. For example, LSU Dental School is requiring students, faculty and staff to be vaccinated or, if they object, to continue to be tested weekly for COVID and continue to wear a mask while in clinic. When requiring vaccinations, employers should ask employees what kinds of support they might need to get the vaccine. A paid day or two off to recuperate may be essential. Hotels and restaurants can facilitate greater vaccine uptake by providing paid time off to the thousands of hospitality workers in New Orleans. Providing the supports needed to ensure all hospitality workers can receive and recuperate from the vaccine could greatly increase vaccine uptake in this industry, which in turn could position New Orleans’ tourism industry very favorably among convention planners and leisure travelers.
Engaging health professionals to proactively reach out to their younger adult patients to provide information about the safety and importance of the vaccine is a strategy that would ensure this group has the information they need to make an informed decision. Concerns and fears should be addressed respectfully and empathetically. Providing multiple, accessible opportunities to get vaccinated will also be helpful, giving individuals time to consider the information provided and confer with family and friends.
COVID extracted a huge price from New Orleans — in lives, lost wages, lost businesses and more. Business leaders could give the city an enormous shot in the arm (pun intended) by doing what it takes to help their workers get vaccinated. The result could be a new New Orleans, quickly competitive with other tourist meccas, and with a new reputation as an equitable destination to boot.
Footnotes and Sources
Zeller, M., Gangavarapu, K., Anderson, C., Smither, A. R., Vanchiere, J. A., Rose, R., … & Andersen, K. G. (2021). Emergence of an early SARS-CoV-2 epidemic in the United States.
The Data Center analysis of Orleans Parish Coroner report.
The Data Center analysis of LDH data
Zeller, M., Gangavarapu, K., Anderson, C., Smither, A. R., Vanchiere, J. A., Rose, R., … & Andersen, K. G. (2021). Emergence of an early SARS-CoV-2 epidemic in the United States.
“COVID-19 Prevalence Study -Jefferson and Orleans Parishes” Ochsner Health, accessed February 2021, htv-prod-media.s3.amazonaws.com/files/7-2-2020-ochsner-health-prevalence-results-deck-final-1593709446.pdf
Basu, A. (2020). “Estimating The Infection Fatality Rate Among Symptomatic COVID-19 Cases In The United States”: Study estimates the COVID-19 infection fatality rate at the U.S. county level. Health Affairs, 39(7), 1229-1236.
Joo, H., Miller, G. F., Sunshine, G., Gakh, M., Pike, J., Havers, F. P., Kim, L., Weber, R., Dugmeoglu, S., Watson, C., & Coronado, F. (2021). “Decline in COVID-19 Hospitalization Growth Rates Associated with Statewide Mask Mandates – 10 States, March-October 2020”. Morbidity and Mortality Weekly Report, 70(6), 212–216. doi.org/10.15585/mmwr.mm7006e2
Tyler Smith, “COVID-19 patient outcomes improve thanks to new medications, top-notch care”, UCHealth Today, accessed February 2021, www.uchealth.org/today/covid-19-care-improvements-include-new-medications-better-treatments/
Dondorp, A. M., Hayat, M., Aryal, D., Beane, A., & Schultz, M. J. (2020). “Respiratory Support in COVID-19 Patients, with a Focus on Resource-Limited Settings”, The American Journal of Tropical Medicine and Hygiene, 102(6), 1191-1197, accessed March 16, 2021, from www.ajtmh.org/view/journals/tpmd/102/6/article-p1191.xml
“FDA Approves First Treatment for COVID-19”, U.S. Food and Drug Administration, accessed February 2021, www.fda.gov/news-events/press-announcements/fda-approves-first-treatment-covid-19
Hutchins, H. J., Wolff, B., Leeb, R., Ko, J. Y., Odom, E., Willey, J., … & Bitsko, R. H. (2020). “COVID-19 mitigation behaviors by age group—United States”, April-June 2020. Morbidity and Mortality Weekly Report, 69(43), 1584.
“Gov. Edwards: Louisiana Will Quickly Implement New Federal Guidance to Expand Nursing Home Visitation”, accessed February 2021, gov.louisiana.gov/index.cfm/newsroom/detail/2694
Nancy Ochieng, Priya Chidambaram, Rachel Garfield, and Tricia Neuman. “Factors Associated With COVID-19 Cases and Deaths in Long-Term Care Facilities: Findings from a Literature Review”, Kaiser Family Foundation, accessed February 2021, www.kff.org/coronavirus-covid-19/issue-brief/factors-associated-with-covid-19-cases-and-deaths-in-long-term-care-facilities-findings-from-a-literature-review/
The Data Center analysis of Census 2010 data.
The Data Center analysis of Orleans Parish Coroner data and Population Estimates 2019.
“A Detailed Map of Who Is Wearing Masks in the U.S.”, NY Times, accessed March 13, 2021, www.nytimes.com/interactive/2020/07/17/upshot/coronavirus-face-mask-map.html
Hearne, B. N., & Niño, M. D. (2021). “Understanding How Race, Ethnicity, and Gender Shape Mask-Wearing Adherence During the COVID-19 Pandemic: Evidence from the COVID Impact Survey.” Journal of Racial and Ethnic Health Disparities, 1-8.
Hearne, B. N., & Niño, M. D. (2021). “Understanding How Race, Ethnicity, and Gender Shape Mask-Wearing Adherence During the COVID-19 Pandemic: Evidence from the COVID Impact Survey.” Journal of Racial and Ethnic Health Disparities, 1-8.
The Data Center analysis of Week 25 Household Pulse Survey
Bunch, L. (2021, January). “A tale of two crises: Addressing Covid-19 vaccine hesitancy as promoting racial justice.” In HEC forum (pp. 1-12). Springer Netherlands.
Silver, V., Chapple, A. G., Feibus, A. H., Beckford, J., Halapin, N. A., Barua, D., … & Clement, M. E. (2020, September). “Clinical Characteristics and Outcomes Based on Race of Hospitalized Patients With COVID-19 in a New Orleans Cohort.” In Open Forum Infectious Diseases (Vol. 7, No. 9, p. ofaa339). US: Oxford University Press.
The Data Center analysis of LDH data
The Data Center analysis of EMSI data
“Everyone in Louisiana ages 16 and older is eligible to get vaccinated against COVID-19.”, Louisiana Department of Health, accessed March 2021, ldh.la.gov/index.cfm/page/4137
The Data Center analysis of EMSI data
“COVID-19 Outbreaks”, Louisiana Department of Health, accessed March 2021, ldh.la.gov/index.cfm/page/3997
“Is your BMI high enough to qualify for a coronavirus vaccine under new rules? Find out here.” The Advocate, accessed March 2021, www.theadvocate.com/baton_rouge/news/coronavirus/article_67b13f74-80f7-11eb-a951-5fae0db68844.html
“Louisiana Widens Vaccine Access for Pre-existing Conditions” Biz New Orleans, accessed March 2021, www.bizneworleans.com/louisiana-widens-vaccine-access-for-pre-existing-conditions/
Blake Paterson. “Louisiana reaches record-low COVID hospitalizations as John Bel Edwards expands vaccine eligibility” The Advocate, accessed March 2021, www.theadvocate.com/baton_rouge/news/politics/legislature/article_b8383448-8804-11eb-b1ef-4feeffdf37a9.html
Jenna Losh and Allison Plyer. “Demographics of New Orleans and early COVID-19 Hot Spots in the U.S.” accessed March 2021, next.datacenterresearch.org/covid-19-data-and-information/demographic-data/
The Data Center analysis of American Community Survey 2019. Table S0802.
The Data Center analysis of American Community Survey 2019. Table S2802.
next.datacenterresearch.org/reports_analysis/who-are-the-essential-workers-keeping-the-new-orleans-region-going/ and next.datacenterresearch.org/covid-19-data-and-information/demographic-data/
Randy Yeip. “As Covid-19 Vaccinations Ramp Up, Hesitancy Wanes”, The Wall Street Journal, accessed April 2021, www.wsj.com/articles/as-covid-19-vaccinations-ramp-up-hesitancy-wanes-11617096603
“Statewide COVID-19 Survey: Vaccine Findings”, Louisiana Public Health Institute, accessed April 2021, lphi.org/wp-content/uploads/2021/04/Covid-Survey-Vaccine-Findings-for-website-1April2021.pdf
“Vaccines and Related Biological Products Advisory Committee Meeting” FDA, accessed March 2021, www.fda.gov/media/146217/download
“Vaccines and Related Biological Products Advisory Committee Meeting” FDA, accessed March 2021, www.fda.gov/media/146217/download and Tara Parker-Pope. “Is the Second Dose Bad? If I Feel OK, Is It Working? Can I Take Tylenol?”, NY Times, accessed April 2021, www.nytimes.com/2021/04/02/well/live/covid-vaccine-side-effects-faq.html?smid=url-share
“City Partners with Uber, Greater New Orleans Foundation, LCMC Health, and Urban League of Louisiana to Provide 20,000 Rides to Vaccine Sites” City of New Orleans, accessed March 2021, nola.gov/mayor/news/march-2021/city-partners-with-uber,-greater-new-orleans-foundation,-lcmc-health,-and-urban-league-of-louisiana/
Kimberly Curth. “New Orleans EMS delivering COVID-19 vaccines to those with medical mobility issues”, New Orleans WVUE, accessed April 2021, www.fox8live.com/2021/03/23/new-orleans-ems-delivering-covid-vaccines-those-with-medical-mobility-issues/
Sarah Ravits. “Coronavirus vaccines with a side of fried fish are on the Good Friday menu in Central City”, The Gambit, accessed April 2021, www.nola.com/gambit/news/the_latest/article_beda26b0-930a-11eb-a638-07e008c82817.html
Blake Paterson. “LSU Dental School backtracks, won’t require COVID vaccines amid concerns over religious liberties”, The Advocate, accessed April 2021, www.theadvocate.com/baton_rouge/news/coronavirus/article_759d3766-8d7a-11eb-80b9-27a368dd9d54.html
Abby Goodnough. “Getting to Yes: A Nursing Home’s Mission to Vaccinate Its Hesitant Staff”, NY Times, accessed April 2021, www.nytimes.com/2021/03/28/health/nursing-home-covid-19-vaccine.html